Your overall health is important to us, and the university offers a variety of benefits to help support your physical and mental health. University of Louisville offers four health plans through Anthem Blue Cross Blue Shield. Yes, a benefit year deductible applies for most medical services accessed outside the student health center .
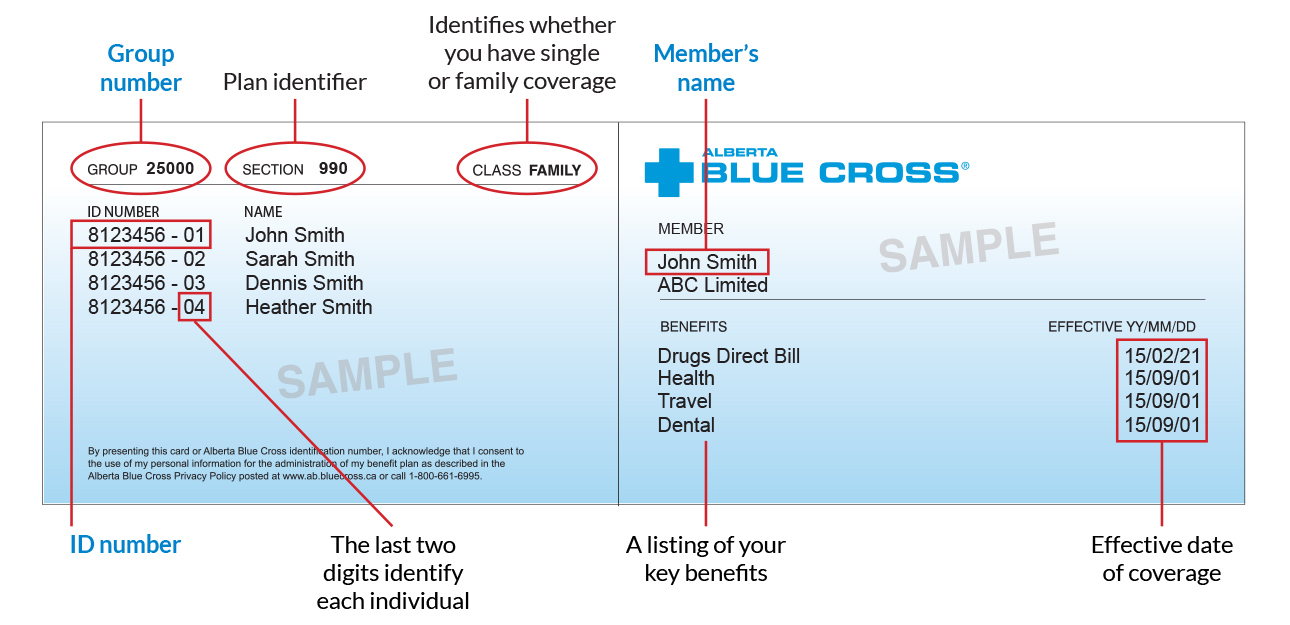
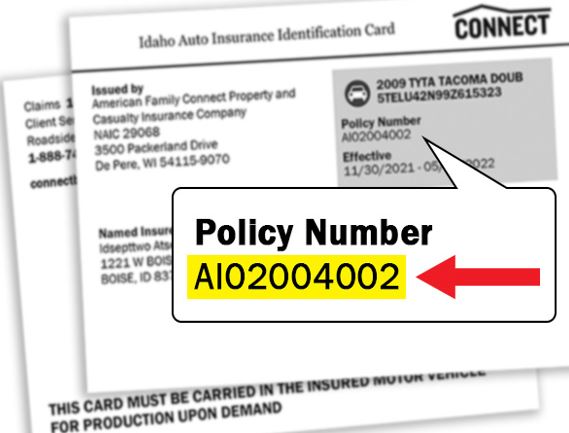
Visit theMy Coverage pageto check your plan's annual deductible. This deductible does not apply to services with fees at an SHC, to emergency or urgent care clinic visits for students, or to pharmacy claims. For some UC SHIP campuses, the benefit year deductible does not apply to UC Family services. If you have questions about the services rendered, you should contact the health care provider. If you have questions, please contact Member Service at the number on the front of your ID card.
Sharp Health Plan continues to be recognized in California and nationally for their high-quality care and service. They are the highest member-rated health plan in California, and they also hold the highest member ratings for health care, personal doctor and specialist among reporting California health plans. As part of Sharp HealthCare's integrated delivery system, Sharp Health Plan directly connects members to an expansive network of nationally recognized doctors, elite-rated medical groups and hospitals. Who we areAnthem, Inc. is one of the largest health benefits companies in the United States. With local service and the value of the Blue Cross brand, we have been committed to ensuring our members have access to affordable health benefits for over 80 years.
Finally, you might see a dollar amount, such as $10 or $25. This is usually the amount of your co-payment, or "co-pay." A co-pay is a set amount you pay for a certain type of care or medicine. Some health insurance plans do not have co-pays, but many do. If you see several dollar amounts, they might be for different types of care, such as office visits, specialty care, urgent care, and emergency room care.
If you see 2 different amounts, you might have different co-pays for doctors in your insurance company's network and outside the network. If you need a service not offered at the SHC, your clinician will refer you to an off-campus health care provider. The SHC will provide you with a referral to see the off-campus provider. This is not a guarantee of payment, and your deductible, copay and coinsurance will apply. Your SHC clinician may suggest a specific provider, or you can choose a provider. However, we strongly recommend that UC SHIP members see providers who belong to the Anthem Blue Cross Prudent Buyer PPO network, including UC Family providers.
Doing so ensures UC SHIP members will pay the lowest out-of-pocket costs. UnitedHealthcare Signature1 - The Signature plan includes our full network of contracted providers. With this HMO plan, members simply choose a primary care physician from our full network of contracted providers to coordinate all their medical care. They can then visit their PCP for routine checkups, and when they need to see a specialist, their PCP provides a referral. Members are charged only a copayment for each doctor's visit.
However, not all small, independent pharmacies have the correct computer system to validate your transaction, in which case you'll need to pay for the prescription using another form of payment. UC SHIP provides 100% coverage of allowed charges for emergency room services after a copayment, and 100% coverage of urgent care center allowed charges after a specified copayment. If Anthem determines that the reason for the visit was not an emergency, the coverage of the charges will be reduced. The annual deductible does not apply to emergency room or urgent care center visits. If you are admitted to the hospital, UC SHIP will cover a percentage of inpatient charges, and the emergency room copayment will be waived. Visit theMy Coverage page to view the benefit levels, copayments and coinsurance for your campus.
All follow-up care must be authorized in advance by the SHC. If possible, try to see the same doctor or nurse practitioner for each visit. Knowing your clinician makes visits more comfortable and helps ensure the best outcome each time.
Because of its large network of providers, giving you many choices for where you get medical services. Anthem has a variety of health insurance plans available including options for individuals, families, Medicare, Medicaid and group insurance. If you do not see your coverage amounts and co-pays on your health insurance card, call your insurance company . Ask what your coverage amounts and co-pays are, and find out if you have different amounts and co-pays for different doctors and other health care providers. When you receive a bill from your doctor, it is often for your copayment, co-insurance, or deductible. These are features of health plans, and basically have the member share in some of the cost of their health care.
For example, some health plans require that the member pay $10 for an office visit and the rest is covered by the plan. You pay 20% of the cost for all specialist office visits after you meet the annual deductible. Your specialist may charge you up to the full amount of your deductible at the time of service, and you may need to file a claim to get reimbursed. You can visit any provider or specialist of your choice without preauthorization from your primary care doctor. Each UC SHIP campus has its own out-of-pocket limits , depending on where you access care. Visit the My Coverage page to review your campus's benefits.
Medical and pharmacy copayments, as well as coinsurance and the deductible, apply toward the out-of-pocket maximum. You will pay a lower out-of-pocket maximum if you receive care from the SHC and network providers. You will pay a higher out-of-pocket maximum if you visit out-of-network providers. Because your PCP coordinates your care, you should always let our group know whenever you seek treatment of any kind.
For further details about the specific cases that don't require a referral, please call Member Service at the number on the front of your ID card. HMO - A Health Maintenance Organization plan provides health care from specific doctors and hospitals under contract with the plan. You pay co-payments for some services, but you have no deductible, no claim forms, and a geographically restricted service area. In 2004, WellPoint Health Networks Inc and Anthem, Inc. merged and became the nation's leading health benefits company. In December 2014 WellPoint Inc. changed its corporate name to Anthem, Inc. Anthem has about 40 million members and is ranked 33rd on the Fortune 500.
WHA offers affordable, quality health care to its neighbors in Marin, Napa, Sacramento, Solano, Sonoma, Yolo and parts of Colusa, El Dorado, Humboldt, and Placer counties. The student health center at each University of California campus gladly offers reciprocal access to currently registered students from all other UC campuses under the same conditions that apply to its own students. If you visit an SHC at another campus, you may need to pay out of pocket and be reimbursed for any services you receive.
Please check with the SHC you plan to visit for more information about fees and filing claims to UC SHIP. The "coverage amount" tells you how much of your treatment costs the insurance company will pay. This information might be on the front of your insurance card. It is usually listed by percent, such as 10 percent, 25 percent, or 50 percent.
For example, if you see 4 different percent amounts, they could be for office visits, specialty care, urgent care, and emergency room care. Also, now Anthem is offering their Blue Card for individual and family plans again. The Blue Card offers some health care services to Blue Cross members while traveling out-of-state. This may give a bit of a competitive edge to Anthem Blue Cross over Blue Shield. However, the main competitive edge of these California health plans, which differs by region, remains the size of the medical provider networks. The MetLife DHMO plans provide access to a large network of dental providers throughout California.
Preventive dental care is an important part of overall health and MetLife is committed to ensuring that its members receive a high level of dental care. As part of this commitment, all Quality Management Activities are designed to meet or exceed NCQA standards. These standards are applied to plan design, through the credentialing of network providers, member services standards and on-going peer review and facility audits. If you use an in-network provider, you don't need to file a claim — your doctor will file one with Anthem. Anthem will then pay your doctor amounts it covers under the Health Account Plan and send you an Explanation of Benefits . Health coverage through Anthem offers access to an extensive network of providers for all your medical, prescription drug and mental health care needs.
The health care network specified by your Anthem insurance policy will determine whether you have access to in-network providers in other states. When submitting an out-of-state claim, you must contact Anthem's customer service department because the process may be different. You might see another list with 2 different percent amounts. Beginning in 2013, Anthem Blue Cross became the behavioral health provider for Anthem HMO and PPO plans. If you are enrolled in one of these Anthem plans, you do not need a referral from your primary care physician in order to receive mental health services.
Visit Anthem's website at /ca for a list of behavioral health providers. When you and your primary care provider determine that you need specialized care, your PCP will "refer" you to a specialized provider from our trusted team. A referral is required by your HMO health plan before the plan will cover certain services.
PPO - A Preferred Provider Organization is similar to a traditional "fee-for-service" plan, but you must use doctors in the PPO provider network or pay higher co-insurance . You must usually meet an annual deductible before some benefits apply. You're responsible for a certain co-insurance amount and the plan pays the balance up to the allowable amount.
Visit your health plan's website to learn how benefits, claims, and payment of claims are covered, as well as the service limitations and exclusions that may apply. You can also log in to myCalPERS to use the Search Health Plans tool to research the health plan coverage and benefits most important to you and your family. UnitedHealthcare of California is committed to providing quality coverage and affordable benefits to help keep you and your family healthy.
Our plans offer more than just doctor visits; preventive care services are also provided for every member of the family. If you use an out-of-network provider, you may need to pay your doctor up front and then file a claim with Anthem. Anthem will then pay your doctor amounts it covers under the HAP and send you an EOB. You need your ID card anytime you visit the student health center on campus or go to a doctor's office, urgent care clinic, hospital, pharmacy, etc. UC SHIP offers a range of benefits, including coverage for specialty office visits, prescriptions, diagnostic services, surgery, hospitalization and out-of-area care while traveling, to name a few.
The UC SHIP package also includes strong dental and vision benefits and covers most SHC fees. It's best to check your health care options before using the emergency room . Plus, when you visit in-network providers, you may pay less for care. Anthem's size has advantages such as being widely recognized and having the financial weight to provide members with good tech tools and helpful medical resources. There are also downsides including poor customer service and a lack of personalization.
Vision Wear coverage is provided through Anthem Blue View Vision. Coverage is included in your enrollment in the medical plan, but vision services have their own schedule of benefits and network providers separate from medical benefits. If you forget or aren't sure what type of health insurance plan you have , you can find out on your BCBS ID card. If you have an HMO, your card may also list the physician or group you've selected for primary care. Determining whether a provider is in-network is an important part of choosing a primary care physician.
Which plan offers the most doctors, hospitals and medical provider networks? Or, more importantly, which plan does your primary care physician or specialist take? At the end of the day, most California consumers care more about whether or not their personal doctor is covered then they care how many doctors are in-network. Each covered member of your family may choose his or her own primary care provider , and choosing the right one is important. There are many different types of PCPs, including general practitioners, internists, pediatricians, family medicine physicians, and nurse practitioners. To choose the best fit for you or your family member, begin by asking for recommendations from the people you trust.
You should also consider each PCP's distance and accessibility from your work or home. Most importantly, talk with us to be sure that the practice can meet your personal health care needs. If your plan doesn't require that you choose a PCP, you can see a specialist or other health care provider without a referral. However, you'll still need to see a provider who participates with Blue Cross Blue Shield of Massachusetts in order to have your benefits covered at the highest level. What's more, we have a clear vision for a healthy Georgia – to help improve the lives of the people we serve and the health of our communities.
We are a team of caring individuals who invest our best ideas and efforts to help create innovative health coverage solutions that are accessible to all Georgians in our service area. We offer customers choice and flexibility in meeting their health plan needs. These options are continually fine-tuned to enhance access to affordable, quality health care coverage. EPO - The Exclusive Provider Organization plan offers the same covered services as an HMO plan, but you must seek services from the plans' PPO network of preferred providers. With a mix of benefits that deliver patient-centered care, health and wellness programs and award-winning customer service, UnitedHealthcare is a smart choice for your family's health care coverage needs. Our Signature plan offers access to a full network of contracted providers with more than 62,590 physicians and health care professionals, and 273 hospitals.
The Advantage, Alliance and Harmony plans offer the same level of benefit coverage as our Signature plan but has a narrower network of contracted providers. You can find listings for physicians and hospitals in our provider directories. With Sutter Health Plus, members gain access to an integrated network of high-quality healthcare providers, including many of Sutter Health's hospitals, doctors and healthcare services. There are also 12-step programs, such as Alcoholics Anonymous and Narcotics Anonymous , which anyone can attend. If you elected the Health Care Flexible Spending Account , the money in your FSA will be used first to reimburse you for any out-of-pocket health care expenses—since the FSA has a "use-it or lose-it" rule.
HealthEquity | WageWorks administers your FSA and will automatically debit your FSA first to pay for any out-of-pocket medical expenses. If you don't have enough in your FSA to cover the expenses, HealthEquity | WageWorks will then debit your Health Account. Examples include, but are not limited to, prosthesis manufacturers, durable medical equipment suppliers, independent or chain laboratories or telemedicine providers. Behavioral health benefits are provided through Anthem Blue Cross. You can see any behavioral health provider you choose, but you'll pay less and receive higher benefit coverage when you see an in-network provider. For services outside the SHC, UC SHIP contracts with Anthem Blue Cross to provide access to its extensive network of hospitals and providers, including UC Family facilities and provider groups.
For routine care, start at the student health center on your campus. When you need medical care, call or visit your campus's SHC website to make an appointment. On most campuses, the SHC will file claims to UC SHIP, so you don't have to bother with the paperwork.
The back or bottom of your health insurance card usually has contact information for the insurance company, such as a phone number, address, and website. This information is important when you need to check your benefits or get other information. For example, you might need to call to check your benefits for a certain treatment, send a letter to your insurance company, or find information on the website. This plan combines traditional medical coverage with a Health Savings Account . Under this plan, all covered services (except preventive services/prescriptions) are subject to the deductible, which must be met before the plan will begin paying its share of the cost of healthcare expenses. However, you can pay for that deductible using the tax-free funds in your HSA.






















No comments:
Post a Comment
Note: Only a member of this blog may post a comment.